The Bingel Laboratory

Prof. Dr. Ulrike Bingel and her research group focuses on the interaction between pain and cognitive processes. We have a longstanding expertise in investigating the CNS mechanisms underlying nociception, pain, and pain modulation in health and disease. In our research, we use behavioural paradigms, pharmacological modulations, as well as functional and structural brain imaging. Being particularly intrigued by the reciprocal effects of pain and cognition, we have a strong focus on translational questions such as the role of expectations and prior experiences on analgesic treatment outcomes. Our interdisciplinary research group comprises neurologists, neuroscientists, psychologists, biologists, and computer scientists and is based at the Department of Neurology at the University Medicine Essen. We are affiliated with the Erwin-L-Hahn institute for magnetic resonance imaging and the Translational Pain Research Department of the University Pain Center. Our research is funded by the Deutsche Forschungsgemeinschaft.
Recent News
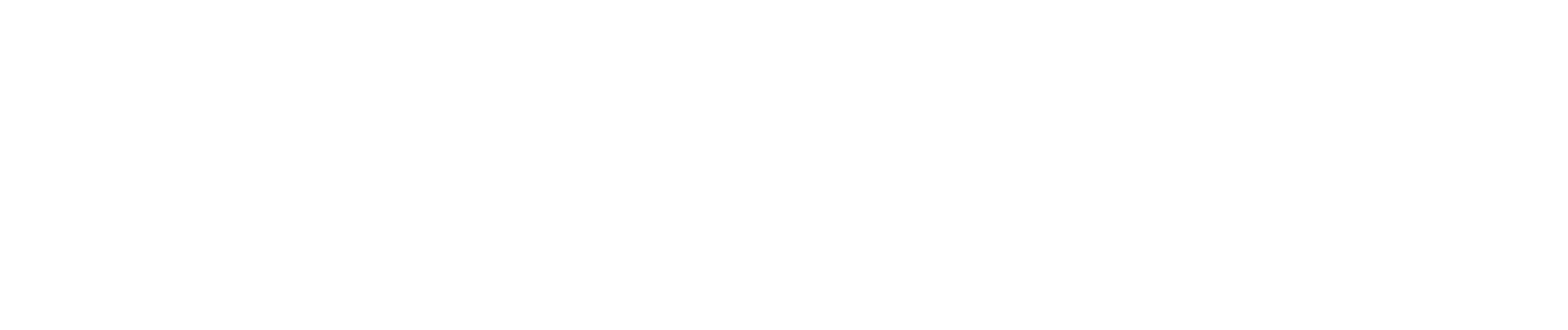
A new study from our team, published in JAMA Network Open (October 2025), shows that open-label placebos (OLPs)—placebos honestly described as such—can meaningfully improve quality of life in people with migraine when added to standard preventive treatment. While OLPs did not reduce headache frequency, patients receiving OLPs reported less pain-related disability and felt significantly better overall. These findings, led by Julian Kleine-Borgmann and Katharina Schmidt, and conducted in collaboration with the Frankfurt Headache Center within the DFG-funded CRC 289 Treatment Expectation, suggest that OLPs may represent an ethical and safe add-on option to enhance patient-centered migraine care. Read the full article in JAMA Network Open
The study “The association between test anxiety, learning strategies, and open-label placebo effects on academic test performance” presents a secondary analysis of a randomized controlled trial. Elisa Frisaldi examined whether test anxiety and individual learning strategies moderate the effects of open-label placebos (OLPs) on academic performance. The results suggest that students with higher levels of test anxiety achieved better exam outcomes in the OLP group compared to the control group. Moreover, cognitive, metacognitive, and resource-related learning strategies appeared to interact with the placebo effect. The authors emphasize the need for further studies to confirm and extend these findings. Read the full publication

It was a great pleasure to have Susanne Becker and Lisa Garcia from Heinrich-Heine-University Düsseldorfin our group meeting today! There new data, planned studies, and a lot of time for discussions about shared interests and potential collaborations! More information on Susanne's research group can be found here.
In the picture from left to right: Katharina Schmidt, Ulrike Bingel, Susanne Becker, Lisa Garcia, Sigrid Elsenbruch, and Adriane Icenhour.
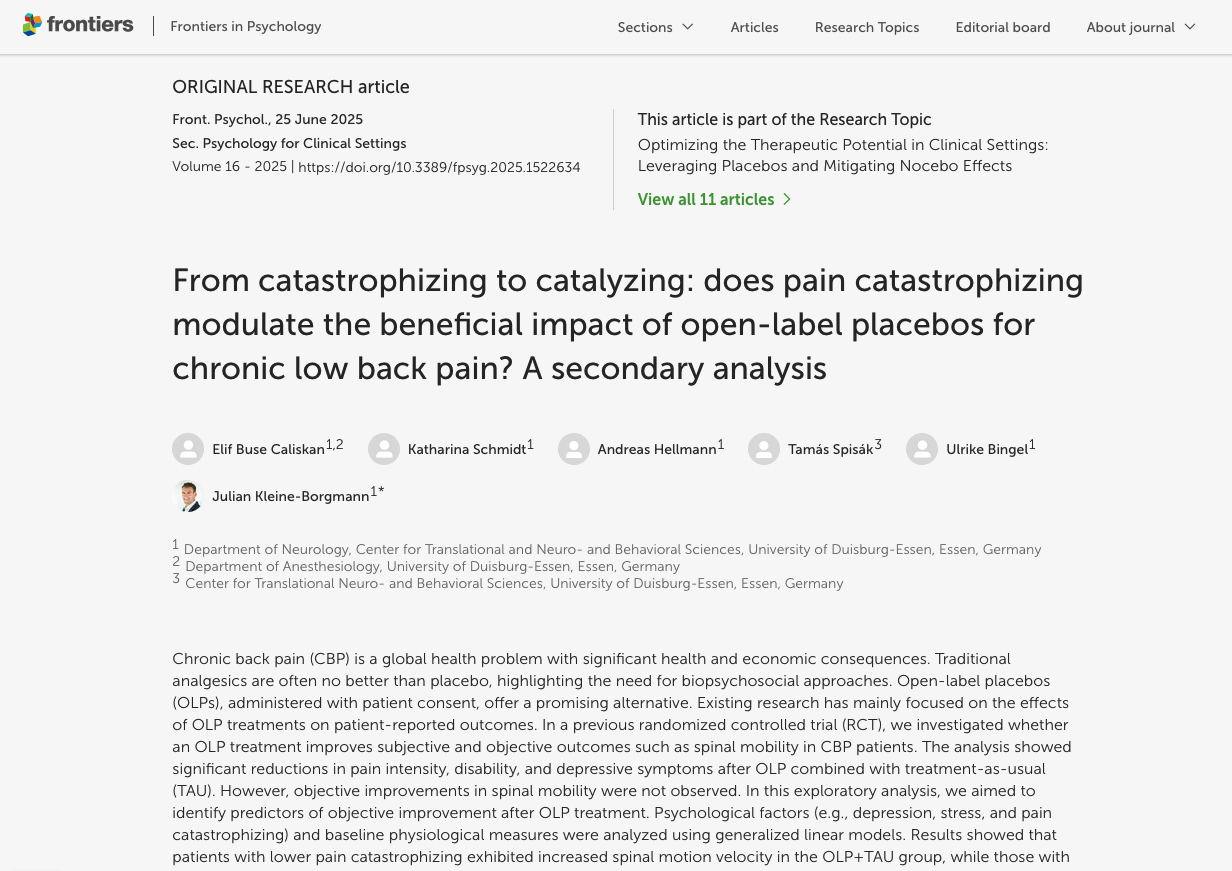
In a recently published exploratory analysis of our randomized controlled trial, Elif Caliskan and members of our team examined whether psychological and physiological factors predict objective improvements (spinal mobility) after OLP treatment combined with treatment-as-usual. The results indicate that patients with lower pain catastrophizing benefited most, showing increased spinal motion velocity, while those with higher catastrophizing did not. These findings highlight that OLPs may provide measurable benefits for specific patient subgroups, pointing toward the potential of personalized pain medicine. Further studies are needed to confirm these results and to better understand the role of psychological factors in chronic pain management. Read the full publication