The Bingel Laboratory Prof. Dr. Ulrike Bingel and her research group focuses on the interaction between pain and cognitive processes. We have a longstanding expertise in investigating the CNS mechanisms underlying nociception, pain, and pain modulation in health and disease. In our research, we use behavioural paradigms, pharmacological modulations, as well as functional and structural brain imaging. Being particularly intrigued by the reciprocal effects of pain and cognition, we have a strong focus on translational questions such as the role of expectations and prior experiences on analgesic treatment outcomes. Our interdisciplinary research group comprises neurologists, neuroscientists, psychologists, biologists, and computer scientists and is based at the Department of Neurology at the University Medicine Essen. We are affiliated with the Erwin-L-Hahn institute for magnetic resonance imaging and the Translational Pain Research Department of the University Pain Center. Our research is funded by the Deutsche Forschungsgemeinschaft. A new (German) podcast episode from the ERCM Medizin Podcast with Ulrike Bingel talks about the power of expectations, its neurobiological mechanisms, doctor-patient communication and the importance of trust in this relationship! Watch the full episode here. Today we have something about science communication! This new (German) book is aimed at healthcare professionals, so everyone working with or around patients: How can you use placebo effects when working with patients? How can you harness the power of expectation in patient care? How can you communicate successfully? Order and read it here as a physical copy or ebook. A new study from our team, published in JAMA Network Open (October 2025), shows that open-label placebos (OLPs)—placebos honestly described as such—can meaningfully improve quality of life in people with migraine when added to standard preventive treatment. While OLPs did not reduce headache frequency, patients receiving OLPs reported less pain-related disability and felt significantly better overall. These findings, led by Julian Kleine-Borgmann and Katharina Schmidt, and conducted in collaboration with the Frankfurt Headache Center within the DFG-funded CRC 289 Treatment Expectation, suggest that OLPs may represent an ethical and safe add-on option to enhance patient-centered migraine care. Read the full article in JAMA Network Open. The study “The association between test anxiety, learning strategies, and open-label placebo effects on academic test performance” presents a secondary analysis of a randomized controlled trial. Elisa Frisaldi examined whether test anxiety and individual learning strategies moderate the effects of open-label placebos (OLPs) on academic performance. The results suggest that students with higher levels of test anxiety achieved better exam outcomes in the OLP group compared to the control group. Moreover, cognitive, metacognitive, and resource-related learning strategies appeared to interact with the placebo effect. The authors emphasize the need for further studies to confirm and extend these findings. Read the full publication
Recent News
Welcome
The Bingel Laboratory
Translational Pain Research Unit
University Medicine Essen
Prof. Dr. Ulrike Bingel
New podcast episode on the placebo effect
New Springer essentials book: The placebo effect explained for healthcare professionals
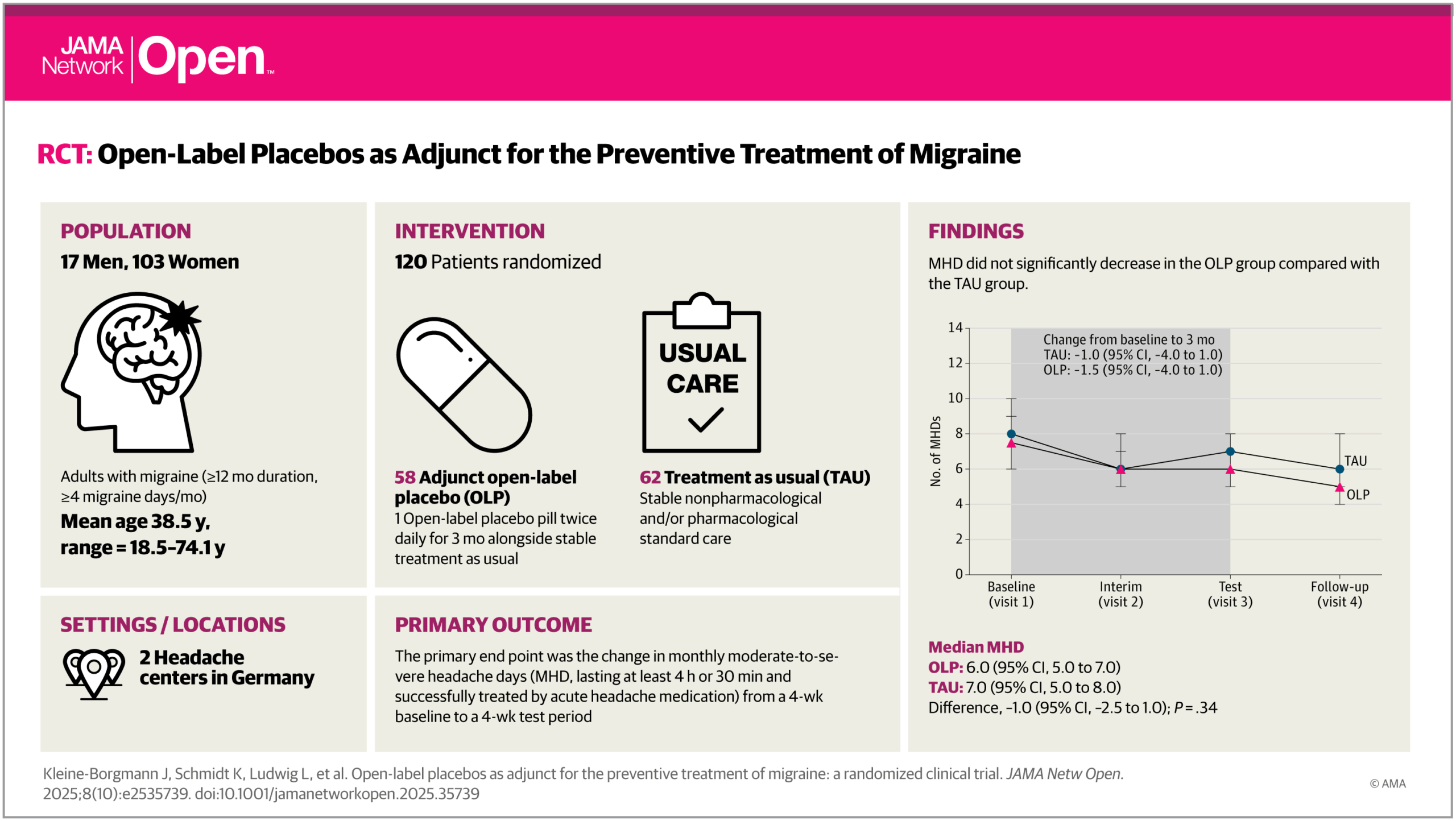
New publication: Open-label placebos as adjunct for migraine prevetion
New publication: Open-label placebos and academic test performance; a secondary analysis.
The Bingel Laboratory
Prof. Dr. med. Ulrike Bingel
Clinical Neurosciences
University Hospital Essen
Department of Neurology
Hufelandstraße 55
45147 Essen
Germany
Fon: +49 (0) 201 723 - 2446
Fax: +49 (0) 201 723 - 6882
Mail: ulrike.bingel@uk-essen.de
Copyright 2021 - Bingel Laboratory